In today’s rapidly evolving global healthcare landscape, market participants encounter a wealth of potential alongside a diverse range of challenges. We understand the importance of negotiating complex and ever-shifting regulations efficiently when structuring cross-border investments and transactions.
In our Guide, you’ll discover invaluable insights to help navigate the dynamic world of healthcare, unlocking opportunities and understanding the developing regulatory landscape.
read more

 Subscribe
Subscribe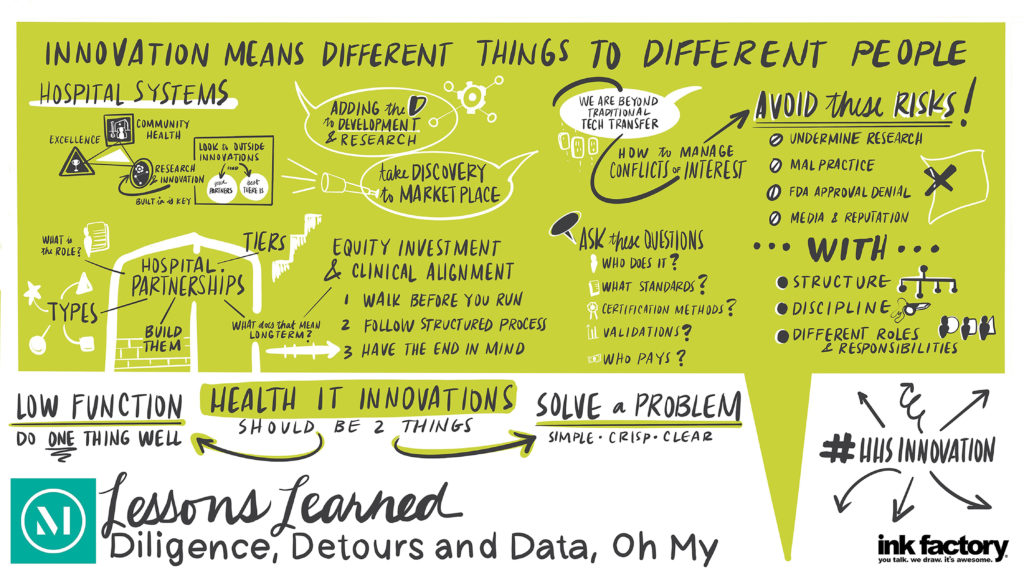
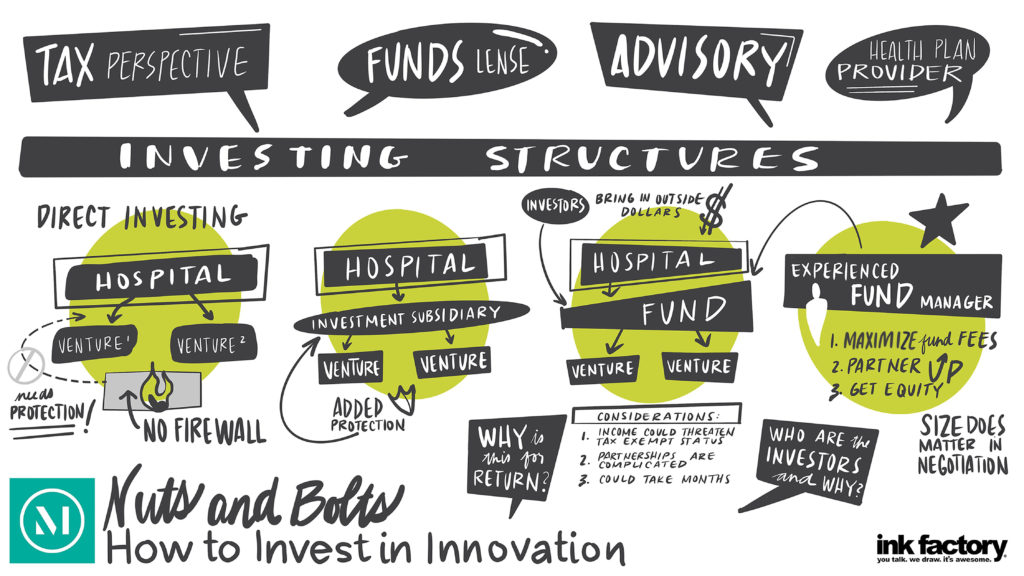 There has been increased interest by hospitals and health systems in creating innovation centers and making innovation center investments, which are helping to transform the healthcare landscape. As they enter this space, hospitals and health systems must first decide how to organize to capitalize on and commercialize innovation opportunities to get innovations into the routine of patient care.
There has been increased interest by hospitals and health systems in creating innovation centers and making innovation center investments, which are helping to transform the healthcare landscape. As they enter this space, hospitals and health systems must first decide how to organize to capitalize on and commercialize innovation opportunities to get innovations into the routine of patient care.